July 29, 2016
In May of 2016, California bill SB 75 officially extended health coverage for low-income undocumented immigrant children 18 years old and younger under what is known as Medi-Cal For All Children.
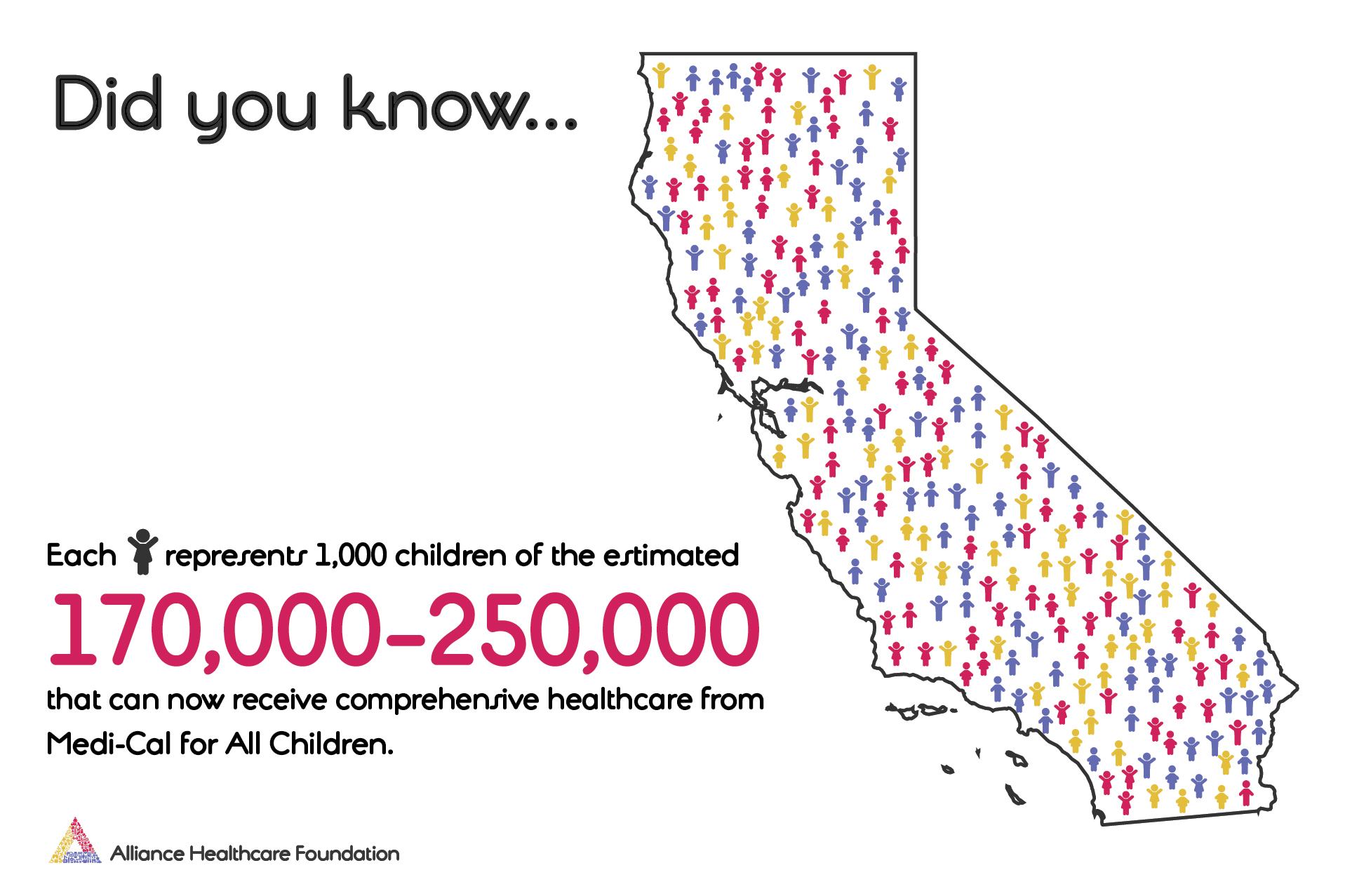
According to reports, the bill will provide comprehensive coverage to between 170,000 and 250,000 undocumented children already receiving limited public health care.
The Department of Health Care Services (DHCS) reports that the state automatically transfers children with “restricted scope” Medi-Cal to “full-scope” Medi-Cal and the children will not have to reapply. Families will receive mail notifications describing their coverage, required enrollment into Medi-Cal managed care and instructions for selecting a health plan and primary care provider.
With full scope comprehensive coverage, children now receive preventive services, primary care, vision, dental, prescription drugs, and specialty mental health and substance abuse services.
While this change represents another critical step towards coverage for all, we must now play an increasingly important role in informing and assisting local families to complete the enrollment process, as required, so that their children will receive all of the care now available.
In a report from Blue Shield of California,the challenges we face informing our communities include:
- Minimal Public Awareness: CHCs noted that unlike the major community media campaigns promoting the ACA expansion, efforts to educate the public about the Medi-Cal for All Children expansion has been much more limited
- Fear Still a Major Issue: Community fear is a pervasive challenge to engaging undocumented and mixed status families in public programs.
- Public Charge Misperceptions: Misperceptions among families, other immigrant service providers (e.g. immigration lawyers) and even county social service agencies about if or how enrolling in Medi-Cal affects existing applications for legal status.
- Indigenous Populations: Mexican and Central American indigenous undocumented residents that speak neither English or Spanish (e.g. Mixteco) are more isolated and the lack of linguistic competence makes serving these residents more difficult.
Community-based organizations (CBOs) and clinics can help communicate that this program is in place, how the managed care model works and the importance of choosing a health plan. It is also important for families to know that Medi-Cal does not share immigration information, and that premium costs may apply if family’s household income is above 160% FPL.
Everyone in the community – community health centers, county Children’s Health Initiatives (CHIs), advocates – can help monitor enrollment and transitions closely to identify new issues affecting families as they arise. For the latest information and assistance, contact your local community clinic or 211 directly.
AHF understands that advancing the health and wellness of children isn’t just the right thing to do, it’s an investment in our future. Please like and share this post to help share this important information.
Related News

Jul 13, 2023
Grants, Pro Bono Consulting & Conferences
Partner News + Opportunities Grants, Pro Bono Consulting and Conferences [...]

Jul 12, 2022
Imperial Valley Wellness Foundation: Opens 2022 Mission Support Applications
Imperial Valley Wellness Foundation Opens Mission Support Funding Application El [...]

Jun 14, 2022
AHF Job Opening
Wanted: Senior Director of Strategy & External Relations and other [...]